History of Nursing and the Need to Innovate
Nurse leaders in Australia recognised the need for innovation within the nursing profession and proposed the establishment of the New South Wales Nurses Association (NSW Branch) in 1949 during mass meetings of nurses at BMA Hall, Macquarie Street, Sydney. At this time there was a severe lack of uniformity in training and skills across the nursing profession and to combat this nurses realised they had to innovate and drive changes in the way education and training was delivered. Their aim was to develop and make available standardised postgraduate courses to teach nurses advanced skills and transform nursing as a profession. The initial courses available at the NSW College of Nursing included the Nurse Administration Diploma, the Industrial Nursing Certificate, and the Sister Tutor Diploma. Innovation and the experience of nurses led to the development of another course and in 1950 the introduction of the Operating Theatre Technique and Management course was added to further advance nursing skills that had previously, not been formally acknowledged.
Another college in Victoria was also established in 1949, the Royal College of Nursing with the same goals, to improve and standardise the nursing profession to drive progress and advancements, regardless of where and by what establishment, training, and medical education was delivered. The NSW College of Nursing changed their name to The College of Nursing in 2003 and in 2012 a federal College of Nursing, the Australian College of Nursing, was formed from the amalgamation of the College of Nursing and Royal College of Nursing, to further reflect uniformity in the training and education of nurses, across Australia. Delivery of courses by lecturers from various establishments including the Medical School and the School of Public Health were gradually replaced with nurse led courses. To ensure all qualifications were standardised, equivalent requirements for registration were established by the General Nursing Council for England and Wales, throughout Austalia and the United Kingdom.
How do Global Challenges Drive Innovation in Nursing?
Nursing faces multiple, global challenges including, the rapid rate of population growth, driven by improvements in healthcare and a significant increase in average lifespan, a recent report conducted by the Australian government stated ‘life expectancy for industrialised countries has risen from 45 to 75 years in the 20th century – and this is largely due to the development of life-saving technologies.’
A few recent articles in the literature have outlined that to meet these requirements sustainably, technological innovation is required to both attract new nurses and deliver training that enables nurses to ‘hit the ground running’.
‘Without innovation, if we deliver health care as we do (with minor tinkering) it is anticipated that health care will consume unsustainable portions of GDP.’
Additionally, the need to innovate is essential to address the challenges of ‘increasing diversity and economic disparity in student populations, shortages of both teachers and clinicians, and concern about the quality and nature of students’ experiences’
The International Council of Nurses Congress in Australia most recent theme was based around global challenges and the future of the nursing industry in Australia. Challenges identified centered around the rise in the aging population, chronic disease, and delivery of universal care for individuals needing long term, mental health support. They investigated the use of innovative technology such as, virtual reality and augmented reality to meet the increased demand for training new nurses to meet the shortfall of nurses which in Australia is ‘expected to reach 85,000 by 2025’
How Will Robots Support Nurses in the Future?
Alongside advancements in the application of virtual reality and augmented reality when delivering medical training, is the potential of robotics in surgery. The application of robotics requires additional training and delivering this via VR or AR is cost effective and has been proven to reduce errors. The International Nursing Association for Clinical Simulation and Learning (INACSL) have recognised the essential need to drive this technology and to encourage a universal approach to practice standards, with simulation training. The INACSL Standards of Best Practice ‘to advance the science of simulation, share best practices, and provide evidence-based guidelines for implementation and training.’
The use of robots as nurses aids is also being researched. One current robotics program taking place at the Duke University Pratt School of Engineering and School of Nursing involves a remote-controlled robot, termed a Tele-Robotic Intelligent Nursing Assistant (TRINA). Students are assessing how a TRINA can provide support for healthcare workers in environments where there is a high risk of infection. Progression of ‘independent’ robots is gaining speed to try to combat the shortage of nurses by providing robots to do tasks that do not require any medical training, thus freeing up nurses to do more clinical and patient centered roles.
How has Innovation within Evidence-Based Practice improved standardised clinical training?
Delivery of standardised clinical training on demand, that can be repeated and analysed, is at the core of innovation within clinically relevant and practical teaching.
‘Evidence based practice is the application of three components.
External evidence includes systematic reviews, randomized control trials, best practice, and clinical practice guidelines that support a change in clinical practice.
Internal evidence includes health care institution based on quality improvement projects, outcome management initiatives, and clinical expertise.
Accounting for patient preferences and values is the third component of this critical equation.’
Evidence-based practice utilising VR and AR enables the evaluation and application of all three components to ensure appropriate treatment is delivered in a time effective way, to improve overall patient outcomes.
What is Happening with Transformation of Medical Education?
Medical education has shifted from theoretical learning with limited ways to apply this in practice, to a stronger focus on providing clinically relevant learning experiences, with VR and AR technology. With VR users can take part in simulations anywhere and repeat them as often as required to achieve the best possible outcomes for the patient.
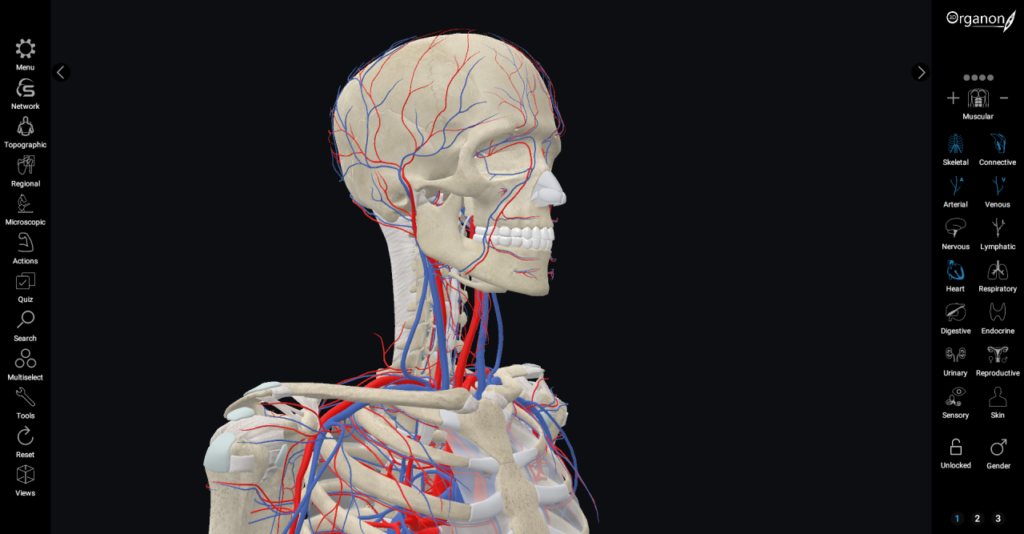
Through the use of immersive technologies to teach anatomy and physiology, and simulation technology, to link imaging to patient assessment, medical education is transforming. Simulation workshops focusing on patient safety provide opportunities to link diagnostics to patient assessment and have developed clinical training based on information provided during an interactive VR simulation. The focus of these training programs include a practical understanding and application of techniques to enhance patient safety, which then generates relevant performance data. This data can then be used to identify gaps in learning and provide additional training using bespoke simulation curricula, created specifically for the user.
An article in the Nursing Times discussed that ‘As VR continues to be implemented and integrated within curricula, its use will become mainstream. The ability for multiple learners to take part in truly interprofessional, completely life-like simulation which is not bound by geography, is set to change how we conduct medical and interprofessional education beyond recognition.’
Applications for Design Thinking and Nurse Led Innovation
Design thinking to identify problems and create prototypes relies on a human-centered approach. DT uses a constructivist approach to drive students to use abductive reasoning, also known as the abductive approach based on creating and testing theoretical hypotheses. Doctors and nurses use abductive reasoning every day, one example would be assessing pathology test results to diagnose a condition.
Associate Professor, Jyothi Marbin, MD at the University of California, San Francisco (UCSF) has been using DT to train medical students and encourage a more creative approach to problem solving and prototyping. Medical educators have traditionally relied on needs assessment techniques when designing curriculum, design thinking differs by prioritising qualitative research and discovery work resulting in the creation of a prototype that is focused on the end user. Still relatively new within medical education DT has been used for over 40 years in other fields, such as Law, although late to be introduced, DT appears to be a valuable tool to drive innovation and create solutions for current and emerging challenges in medical education.
Where is the Current use of Virtual reality and Augmented reality in Medical Education and Training Happening?
Virtual reality and Augmented reality in Medical Education and Training is still relatively new, current use of this technology since 2018, has been extremely effective at the IUPUC Simulation Center based at the Indiana University School of Nursing. VR simulation is combined with high-fidelity mannequins and actors who play the role of patients. Student Nurses can practice skills such as, IV and catheter insertion during a simulation, as well as learning how to diagnose and treat a patient in various situations.
“While actual clinical exposure is fantastic, we can’t create a situation there,” she said. “This technology allows us the flexibility to place it in the curriculum and cater to the needs of our students.”
Shannon Love, clinical assistant professor and director of the simulation center.
Virtual Reality (VR) simulation has also been introduced at the University of New England, School of Nursing. During VR simulations, student nurses interact with acutely ill virtual patients with a variety of conditions including sepsis, heart failure, and respiratory disorders; an immersive, virtual reality setting to learn essential clinical decision-making skills. Students can learn how to communicate and provide support, diagnosis, and treatment for virtual patients without the pressure of knowing a wrong diagnosis or incorrect treatment could result in loss of life. sepsis, pneumonia, heart failure, and meningitis. During the VR simulation, the software monitors actions and records them to compare to best practice. The student can then access a comprehensive data analytics report to find out how they performed and if there are any gaps in their knowledge or skills.
In hospitals, AR is being used to provide a guide by projecting images of the patient’s anatomy onto their skin. One example of this has been pioneered by AccuVein, AR is used to project a patient’s veins onto their skin to help the healthcare workers quickly and easily find a vein, when inserting a needle or a cannula.
In Jersey, St Helier, the Allan Lab, an immersive digital health technologies research laboratory uses VR to enable students to study Cardiology. Dr Andrew Mitchell, a consultant cardiologist, said that,
“The main focus of our research is to explore emerging digital health technologies to advance the understanding of heart conditions and to also provide immersive simulation, procedural training and medical education.”
The COVID-19 pandemic has increased the need for doctors and nurses in addition to demanding skills that they may not be familiar within the medical specialty they are normally working in.
The use of VR in medical education and training has grown rapidly over the past 2 years and is now drawing interest from companies, such as Apple and IBM. It is now anticipated that expeditious technological advancements and with global challenges increase the demand for simulation training will mean VR will be a standard part of training for medical professionals within 5 years.
One ‘report by Grand View Research predicts this market to grow to a whopping $5.1 billion by 2025.’
Is Blockchain Technology the Security Solution for Healthcare Data Security?
Data breaches are a serious issue for healthcare data security and the solution could very well be the utilisation of blockchain technology. Blockchain provides both encryption and validation and prevents data from being altered by storing it in a distributed database, on multiple computers. Users store data in ‘blocks’, each block is timestamped and linked to the previous block of data to form a blockchain in a synchronized database. This becomes almost impossible to hack and provides a secure and economic way to store healthcare data, whilst providing a means for multiple users to access this information seamlessly. Blockchain also provides real-time monitoring of data, providing users access to synchronized databases, with each user having a private key which generates a signature to verify that the data has been input by the user, and protect information from being hacked or altered once it has been signed.
Blockchain technology has several different applications in the healthcare industry. One, in particular, is the way nurses can access and store data which impacts how patient care is coordinated.
‘The regular and updated exchange of a patient’s health and social history will allow nurses to advance the process of discharging patients and data sharing in the continuity of care, the consequence of which is reduced bureaucratic red-tape and an improved quality of nursing interventions, which are crucial in terms of decreasing the unmet needs of patients and citizens.’
Nurses will continue to drive the design and use of new technology to improve efficiency and success during patient treatment. Currently, innovative measures include, ways to further increase the service potential of nurse practitioners; are being reviewed by the Australian College of Nursing, with the aim ‘to develop and deliver health care both within and beyond the hospital; to reimagine health service across a range of contexts.’